Table Of Contents
1. Introduction: The Evolution of Healthcare IT
Healthcare information technology has undergone a remarkable transformation over the past two decades. What began as digitized record-keeping systems has evolved into sophisticated platforms capable of predictive analytics, automated diagnostics, and real-time clinical decision support. Traditional healthcare IT systems—built primarily for administrative efficiency and data storage—are now facing a paradigm shift as artificial intelligence reshapes how medical data is processed, analyzed, and applied.
The adoption of AI in healthcare IT isn't just an incremental upgrade; it represents a fundamental reimagining of how technology supports clinical care. While traditional systems have served as the backbone of healthcare operations, their limitations in handling complex data analysis, predictive modeling, and rapid decision-making have become increasingly apparent. For healthcare professionals and IT decision-makers, understanding the distinctions between AI-driven and traditional healthcare IT systems is essential for strategic planning and competitive positioning in an increasingly data-driven medical landscape.
2. What Are Traditional Healthcare IT Systems?
Traditional healthcare IT systems encompass the foundational digital infrastructure that has supported healthcare operations for decades. These systems include Electronic Medical Records (EMRs), Electronic Health Records (EHRs), Hospital Information Systems (HIS), Laboratory Information Systems (LIS), and Picture Archiving and Communication Systems (PACS).
At their core, traditional systems were designed to digitize paper-based processes, centralize patient information, and facilitate basic administrative workflows. They excel at storing structured data, managing billing and coding, scheduling appointments, and maintaining regulatory compliance documentation. However, these systems operate primarily as sophisticated databases with rule-based logic rather than intelligent platforms capable of learning and adapting.
2.1 Key Limitations of Traditional Healthcare IT Systems:
- Manual data entry and interpretation: Clinical staff must manually input, review, and interpret data, creating bottlenecks and increasing the risk of human error
- Data silos and interoperability challenges: Different systems often cannot communicate effectively, trapping valuable information in isolated databases
- Limited analytical capabilities: Traditional systems provide historical data but lack predictive insights or pattern recognition beyond basic reporting
- Reactive rather than proactive: These platforms respond to queries but cannot anticipate clinical needs or identify emerging patient risks
- Rigid workflows: Pre-programmed rules and processes struggle to adapt to unique patient circumstances or new clinical evidence
- Slow decision-making support: Clinicians must manually search through records and guidelines to inform treatment decisions
- Resource-intensive maintenance: Legacy systems require significant IT support for updates, customization, and troubleshooting
3. AI in Healthcare IT Systems: The New Paradigm
AI-driven healthcare IT systems represent a fundamental departure from traditional approaches by incorporating machine learning algorithms, natural language processing, deep learning neural networks, and predictive analytics into the clinical workflow. Rather than simply storing and retrieving data, AI systems actively analyze information, identify patterns, generate insights, and support clinical decision-making in real time.
These intelligent platforms leverage big data to continuously learn from millions of patient encounters, research studies, and clinical outcomes. They can process unstructured data—such as physician notes, medical imaging, and patient narratives—extracting meaningful insights that would be impossible for traditional systems to capture. AI in healthcare IT transforms data from a passive resource into an active participant in patient care.
3.1 Real-World Applications of AI Healthcare IT:
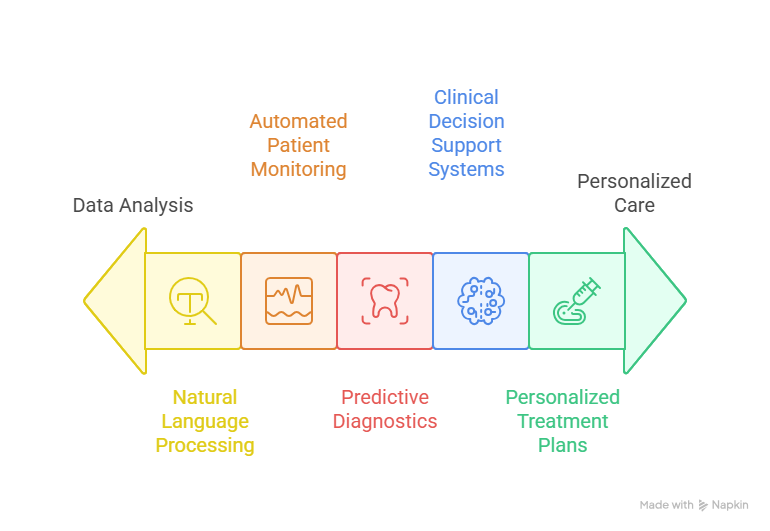
Clinical Decision Support Systems (CDSS): AI-powered CDSS analyze patient data against vast medical knowledge bases to suggest diagnoses, recommend treatments, and flag potential drug interactions or contraindications with greater accuracy than rule-based systems.
Automated Patient Monitoring: Machine learning algorithms continuously analyze vital signs, laboratory results, and clinical notes to predict patient deterioration hours before traditional warning systems would trigger alerts.
Predictive Diagnostics: Deep learning models can detect diseases from medical imaging with accuracy matching or exceeding specialist physicians, identifying subtle patterns in X-rays, CT scans, and pathology slides.
Natural Language Processing: AI systems extract structured insights from unstructured clinical notes, research literature, and patient communications, making vast amounts of previously inaccessible information actionable.
Personalized Treatment Plans: Machine learning algorithms analyze individual patient characteristics, genetic profiles, and treatment responses to recommend highly personalized therapeutic approaches.
4. Key Differences Between AI and Traditional Healthcare IT
Understanding the fundamental distinctions between these two approaches is critical for healthcare organizations evaluating their technology strategy.
4.1 Data Processing and Analysis
Traditional Systems: Process structured data through predefined rules and queries. Analysis is limited to historical reporting and basic statistical functions. Requires manual interpretation of complex patterns.
AI Systems: Process both structured and unstructured data simultaneously. Identify complex patterns, correlations, and anomalies across millions of data points. Provide predictive analytics and risk stratification automatically.
4.2 Decision-Making Speed
Traditional Systems: Clinicians must manually search records, review guidelines, and synthesize information. Decision support is limited to alerting based on predetermined thresholds.
AI Systems: Provide real-time clinical recommendations based on comprehensive analysis of patient data, current research, and best practices. Alerts are contextualized and prioritized based on actual risk.
4.3 Error Reduction
Traditional Systems: Reduce errors related to legibility and information availability but cannot detect clinical reasoning errors or identify subtle patterns indicating patient deterioration.
AI Systems: Actively identify potential diagnostic errors, predict adverse events, flag inconsistencies in treatment plans, and detect early warning signs of complications.
4.4 Personalization of Care
Traditional Systems: Support population-based protocols and standard treatment pathways. Customization requires manual clinician intervention.
AI Systems: Automatically adjust recommendations based on individual patient characteristics, genetic factors, social determinants of health, and real-time response to treatment.
4.5 Scalability and Adaptability
Traditional Systems: Scaling requires significant infrastructure investment. Updates to clinical protocols require manual programming and testing across the system.
AI Systems: Scale horizontally by processing more data to improve accuracy. Continuously learn from new clinical evidence and outcomes without manual reprogramming.
5. Benefits of AI Over Traditional Systems
The advantages of AI-driven healthcare IT extend across clinical, operational, and financial dimensions, creating compelling value propositions for healthcare organizations.
5.1 Clinical and Operational Advantages:
- Improved patient outcomes: AI systems reduce diagnostic errors by up to 30% in some specialties, enabling earlier intervention and more accurate treatment selection
- Enhanced operational efficiency: Automated workflows and intelligent scheduling reduce administrative burden, allowing clinicians to spend more time on direct patient care
- Significant cost reduction: Predictive analytics optimize resource allocation, reduce unnecessary testing, prevent hospital readmissions, and minimize adverse events that generate additional costs
- Real-time clinical insights: Continuous monitoring and analysis provide immediate alerts about patient deterioration, medication interactions, or treatment complications
- Accelerated research and innovation: AI platforms can analyze clinical trial data, identify patient cohorts, and discover new treatment patterns faster than traditional methods
- Population health management: Machine learning identifies at-risk populations and enables proactive intervention programs that prevent disease progression
- Reduced clinician burnout: Automated documentation, intelligent workflow optimization, and decision support reduce cognitive load and administrative tasks
6. Challenges of AI in Healthcare IT
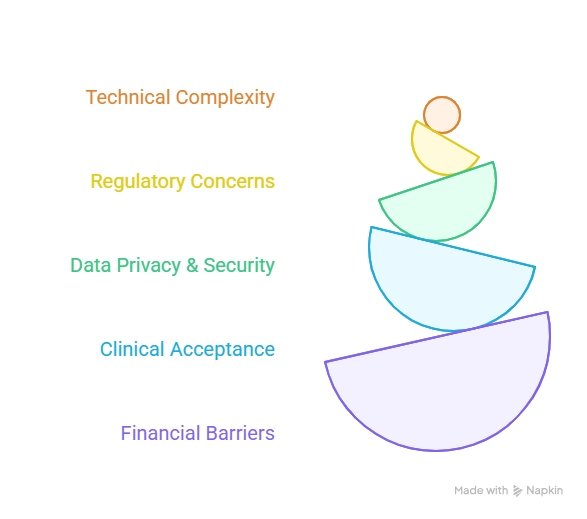
Despite its transformative potential, AI adoption in healthcare IT faces significant hurdles that organizations must address strategically.
The implementation challenge begins with technical complexity. Integrating AI systems with existing legacy infrastructure requires substantial investment in data architecture, interoperability standards, and system redesign. Many healthcare organizations struggle with fragmented data sources, inconsistent data quality, and inadequate IT infrastructure to support computationally intensive machine learning models.
Regulatory concerns present another significant barrier. Healthcare AI systems must comply with HIPAA, FDA approval processes for clinical decision support, and evolving regulations around algorithmic transparency and accountability. The "black box" nature of some deep learning models raises questions about clinical liability when AI recommendations lead to adverse outcomes.
Data privacy and security concerns are amplified in AI systems that aggregate vast amounts of sensitive patient information. Ensuring that machine learning models don't inadvertently expose protected health information or create new vulnerabilities requires sophisticated encryption, access controls, and monitoring systems.
Clinical acceptance remains a critical challenge. Physicians and nurses must trust AI recommendations enough to integrate them into clinical workflows, which requires transparent explanations of how algorithms reach conclusions, validation of accuracy across diverse patient populations, and demonstrated improvements in outcomes.
Financial barriers include high upfront costs for AI platform implementation, ongoing expenses for data scientists and AI specialists, and uncertain return-on-investment timelines that make budget justification difficult for resource-constrained healthcare organizations.
7. Future Outlook: The Convergence of AI and Healthcare IT
The future of healthcare IT lies not in choosing between AI and traditional systems but in their strategic integration. Healthcare organizations are increasingly adopting hybrid approaches that augment existing EHR and HIS platforms with AI-powered modules for specific clinical and operational functions.
Several trends are shaping this evolution. Cloud-based AI platforms are democratizing access to advanced analytics, allowing smaller healthcare organizations to leverage sophisticated machine learning without massive infrastructure investments. Federated learning approaches enable AI models to learn from distributed datasets without centralizing sensitive patient information, addressing privacy concerns while improving algorithm accuracy.
Explainable AI (XAI) technologies are emerging to make algorithmic decisions more transparent and interpretable for clinicians, addressing the black box problem that has hindered clinical acceptance. These systems provide clear reasoning chains that show how patient data, clinical evidence, and algorithmic logic combine to generate recommendations.
Regulatory frameworks are maturing to provide clearer guidance on AI validation, approval, and monitoring in clinical settings. The FDA's evolving approach to adaptive AI algorithms and the European Union's AI Act are establishing standards that will facilitate broader AI adoption while protecting patient safety.
The healthcare workforce is also adapting, with medical education increasingly incorporating data science, AI literacy, and computational thinking alongside traditional clinical training. This cultural shift will accelerate AI integration as a new generation of clinicians enters practice comfortable with AI-augmented decision-making.
Looking ahead, the distinction between "AI systems" and "traditional systems" will likely blur as artificial intelligence becomes a standard feature of all healthcare IT platforms. The question for healthcare leaders isn't whether to adopt AI, but how quickly they can strategically integrate intelligent technologies while managing the associated risks and change management challenges.
8. Frequently Asked Questions
What are the main differences between AI and traditional healthcare IT systems?
The fundamental difference lies in their approach to data and decision-making. Traditional healthcare IT systems function primarily as sophisticated databases that store, organize, and retrieve patient information based on predefined rules. They require manual interpretation and analysis by clinical staff. In contrast, AI-driven systems actively analyze data, identify patterns, generate predictive insights, and provide intelligent recommendations. AI systems learn continuously from new data, adapt to emerging clinical evidence, and can process unstructured information like clinical notes and medical images, capabilities that traditional systems lack.
Can AI completely replace traditional healthcare IT?
AI will not completely replace traditional healthcare IT systems in the foreseeable future, nor should it. Traditional EHR and HIS platforms provide essential foundational capabilities for data storage, regulatory compliance, billing, and basic clinical workflows that remain necessary. The optimal approach is integration, where AI enhances traditional systems with advanced analytics, predictive capabilities, and intelligent decision support. Healthcare organizations will continue to rely on traditional infrastructure while strategically deploying AI for specific high-value applications like diagnostic support, patient risk stratification, and operational optimization.
How does AI improve patient care outcomes?
AI improves patient outcomes through multiple mechanisms. Predictive analytics identify patients at risk of deterioration hours or days before traditional warning signs appear, enabling proactive intervention. Diagnostic AI reduces errors by providing second opinions and detecting subtle patterns that humans might miss. Personalized treatment recommendations based on individual patient characteristics and genetic profiles improve therapeutic effectiveness. Automated monitoring systems ensure that critical changes in patient status are immediately flagged for clinical attention. Additionally, AI optimizes resource allocation, reducing wait times and ensuring patients receive timely care, all of which contribute to better clinical outcomes.
What is the typical implementation timeline for AI healthcare IT systems?
Implementation timelines vary significantly based on organizational readiness, scope of deployment, and system complexity. Pilot projects for specific AI applications like radiology interpretation or readmission prediction can be deployed in 3-6 months. Enterprise-wide AI integration with existing EHR systems typically requires 12-24 months for planning, infrastructure preparation, integration, testing, and clinical validation. However, achieving full clinical adoption and realizing substantial ROI often extends to 3-5 years as organizations iterate on workflows, refine algorithms, and scale successful pilots across departments. Organizations with mature data governance, strong IT infrastructure, and executive sponsorship can accelerate these timelines.
What are the primary data requirements for implementing AI in healthcare IT?
Successful AI implementation requires high-quality, comprehensive datasets that represent diverse patient populations. Minimum requirements include structured clinical data (demographics, diagnoses, procedures, medications, laboratory results) covering thousands to millions of patient encounters. For advanced applications, organizations need unstructured data like clinical notes, radiology reports, and imaging studies. Data must be standardized, clean, and properly labeled for supervised learning applications. Critically, data governance frameworks must ensure privacy protection, appropriate consent, and compliance with regulatory requirements. Organizations should also establish processes for continuous data quality monitoring and algorithm retraining as clinical practices and patient populations evolve.
9. Conclusion: Making the Strategic Choice
The comparison between AI and traditional healthcare IT systems isn't about declaring a winner—it's about recognizing an inevitable evolution. Traditional systems have provided the essential foundation for digital healthcare, but AI represents the next frontier in clinical excellence and operational efficiency. Healthcare organizations that strategically integrate AI capabilities while maintaining robust traditional infrastructure will be best positioned to deliver superior patient outcomes, support their clinical workforce, and remain competitive in an increasingly data-driven healthcare environment.
The question for healthcare leaders is no longer whether to adopt AI, but how quickly and strategically they can implement it. Those who act decisively today will define the standard of care for tomorrow.
Ready to transform your healthcare IT infrastructure? Understanding the distinctions between AI and traditional systems is the first step toward making informed technology investments that drive measurable improvements in patient care and organizational performance.