Table Of Contents
1. Introduction
Medical imaging has long served as the cornerstone of modern diagnostics, enabling healthcare professionals to visualize internal structures and identify pathological conditions. However, the interpretation of medical images—whether X-rays, CT scans, MRIs, or ultrasounds—has traditionally relied heavily on radiologist expertise and is subject to human limitations such as fatigue, cognitive biases, and variability in experience. The integration of artificial intelligence in healthcare, particularly deep learning algorithms, is fundamentally transforming this landscape.
AI in medical imaging represents one of the most promising applications of machine learning in healthcare, offering unprecedented capabilities in pattern recognition, diagnostic precision, and workflow optimization. Deep learning models, especially convolutional neural networks (CNNs), have demonstrated remarkable proficiency in analyzing complex medical images, often matching or exceeding human-level performance in specific diagnostic tasks. This technological evolution is not merely augmenting radiologist capabilities—it is reshaping the entire diagnostic paradigm, making healthcare more accessible, efficient, and accurate.
As healthcare systems worldwide grapple with increasing patient volumes, radiologist shortages, and the demand for faster diagnostic turnaround times, AI-powered medical imaging solutions are emerging as critical tools for addressing these systemic challenges while improving patient outcomes.
2. The Technology Behind AI Medical Imaging
2.1 Deep Learning Fundamentals in Radiology
Deep learning, a subset of artificial intelligence, employs neural networks with multiple layers to automatically learn hierarchical representations of data. In medical imaging, convolutional neural networks have proven particularly effective because they can identify spatial patterns and features within images without explicit programming. These networks learn through exposure to vast datasets of labeled medical images, progressively refining their ability to detect abnormalities, segment anatomical structures, and classify pathological conditions.
The training process involves feeding the algorithm thousands or millions of medical images alongside expert annotations. Through iterative learning cycles, the AI system develops sophisticated pattern recognition capabilities, learning to distinguish between healthy tissue and various disease presentations. Advanced architectures such as ResNet, U-Net, and DenseNet have been specifically adapted for medical imaging applications, each offering unique advantages for different diagnostic tasks.
2.2 Computer Vision and Image Analysis
Computer vision technologies enable AI systems to interpret visual information from medical images with remarkable precision. These systems can perform multiple functions simultaneously: detecting lesions, measuring tissue volumes, tracking disease progression, and identifying subtle abnormalities that might escape human observation. The pixel-level analysis capabilities of deep learning models allow for quantitative assessments that provide objective, reproducible measurements—a significant advancement over qualitative human interpretation alone.
3. Real-World Applications Transforming Patient Care
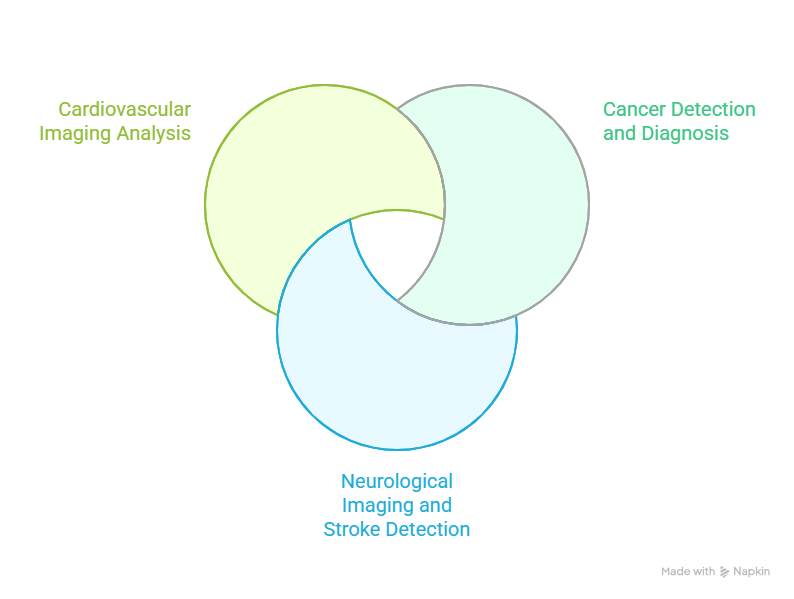
3.1 Cancer Detection and Diagnosis
AI in medical imaging has demonstrated exceptional performance in oncology, particularly in breast cancer screening, lung nodule detection, and skin cancer identification. Studies have shown that deep learning algorithms can detect breast cancer in mammograms with sensitivity rates comparable to or exceeding expert radiologists. In lung cancer screening, AI systems can identify suspicious nodules in CT scans with high accuracy while reducing false-positive rates that often lead to unnecessary biopsies and patient anxiety.
One landmark study published in Nature demonstrated that an AI system could outperform six radiologists in breast cancer detection, reducing false negatives by 9.4% and false positives by 5.7%. Such improvements translate directly into earlier cancer detection, more timely interventions, and ultimately, improved survival rates for patients.
3.2 Neurological Imaging and Stroke Detection
Time-critical conditions like acute ischemic stroke require rapid diagnosis to facilitate timely intervention. AI algorithms can analyze brain CT and MRI scans within minutes, identifying stroke indicators such as intracranial hemorrhage or large vessel occlusions. This rapid triage capability enables healthcare teams to mobilize appropriate resources immediately, significantly reducing the time from imaging to treatment—a critical factor in minimizing brain damage and improving patient outcomes.
AI systems are also proving valuable in detecting early signs of neurodegenerative diseases such as Alzheimer's, identifying subtle structural changes in the brain that may precede clinical symptoms by years. This early detection capability opens new possibilities for preventive interventions and clinical trial recruitment.
3.3 Cardiovascular Imaging Analysis
Cardiac imaging benefits substantially from AI integration, with algorithms capable of automated measurement of cardiac function parameters, detection of coronary artery disease, and risk stratification for adverse cardiovascular events. Deep learning models can analyze echocardiograms to assess ejection fraction, identify wall motion abnormalities, and detect valvular heart disease with high precision.
In coronary CT angiography, AI systems can automatically segment coronary arteries, quantify stenosis severity, and predict the functional significance of lesions—tasks that traditionally require significant radiologist time and expertise. This automation not only improves efficiency but also standardizes measurements across different operators and institutions.
4. Clinical Benefits and Impact on Healthcare Delivery
4.1 Enhanced Diagnostic Accuracy
The primary advantage of AI in medical imaging lies in its ability to improve diagnostic accuracy. Deep learning algorithms excel at identifying subtle patterns and anomalies that may be difficult for human observers to detect, particularly in complex or ambiguous cases. By serving as a "second reader," AI systems can reduce diagnostic errors, catch findings that might otherwise be missed, and provide quantitative assessments that support clinical decision-making.
Research indicates that AI-assisted interpretation can reduce false-negative rates in screening programs while simultaneously decreasing false-positive findings that lead to unnecessary follow-up procedures. This dual benefit enhances both patient safety and healthcare system efficiency.
4.2 Workflow Optimization and Efficiency
Radiology departments face mounting pressure from increasing imaging volumes and persistent workforce shortages. AI solutions address these challenges by automating routine tasks, prioritizing urgent cases, and reducing the time required for image interpretation. Algorithms can perform initial image triage, flagging critical findings for immediate attention while allowing less urgent cases to follow standard workflows.
Automated image analysis also eliminates time-consuming manual measurements and calculations, allowing radiologists to focus on complex interpretations and patient consultations. Studies suggest that AI integration can reduce interpretation time by 30-50% for certain imaging procedures, substantially increasing departmental throughput without compromising quality.
4.3 Standardization and Consistency
Human interpretation of medical images inherently involves some degree of subjectivity and inter-observer variability. AI systems provide consistent, reproducible analyses regardless of time of day, workload pressures, or individual experience levels. This standardization is particularly valuable in multi-center clinical trials, longitudinal disease monitoring, and quality assurance programs.
5. Challenges and Considerations
5.1 Data Quality and Algorithm Training
The performance of AI systems depends critically on the quality and diversity of training data. Algorithms trained on datasets lacking demographic diversity may perform poorly on underrepresented populations, potentially exacerbating existing healthcare disparities. Ensuring that training datasets reflect real-world patient populations across different ages, ethnicities, and clinical presentations remains an ongoing challenge.
Additionally, labeled medical imaging datasets require expert annotations, which are time-consuming and expensive to produce. The medical imaging AI community continues to work on techniques such as transfer learning, semi-supervised learning, and synthetic data generation to address these limitations.
5.2 Regulatory and Integration Challenges
AI medical imaging solutions must navigate complex regulatory pathways before clinical deployment. Regulatory agencies are still developing frameworks to evaluate AI systems that may continue learning and evolving after approval. Integration with existing hospital information systems, picture archiving and communication systems (PACS), and clinical workflows presents technical and organizational challenges that require careful planning and change management.
Healthcare institutions must also address questions of liability, quality assurance, and clinical validation when implementing AI solutions. Clear protocols for human oversight, system monitoring, and performance auditing are essential to ensure patient safety and maintain trust in AI-assisted diagnostics.
5.3 The Human Element in AI-Assisted Radiology
Despite impressive capabilities, AI systems are tools that augment rather than replace human expertise. Radiologists provide essential clinical context, correlate imaging findings with patient history and other diagnostic information, and communicate results to referring physicians and patients. The future of radiology lies in collaborative intelligence—leveraging AI's pattern recognition capabilities alongside human clinical judgment, contextual understanding, and empathetic patient care.
6. The Future of AI in Medical Imaging
6.1 Emerging Technologies and Innovations
The next generation of AI medical imaging solutions will likely incorporate multimodal learning, integrating imaging data with electronic health records, genomic information, and other clinical data sources to provide more comprehensive diagnostic insights. Explainable AI techniques are being developed to make algorithm decisions more transparent and interpretable, addressing concerns about "black box" decision-making in clinical contexts.
Federated learning approaches promise to enable AI model training across multiple institutions without sharing sensitive patient data, potentially creating more robust and generalizable algorithms while maintaining privacy protections. Real-time AI guidance during imaging procedures could optimize image acquisition and reduce the need for repeat scans.
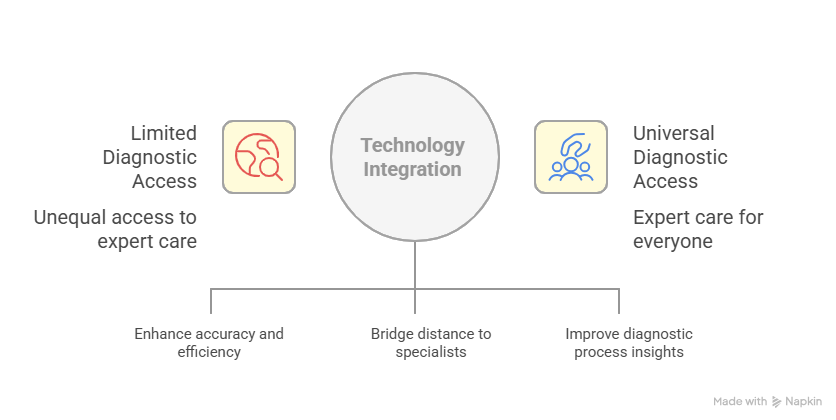
6.2 Expanding Access to Expert-Level Diagnostics
Perhaps the most transformative potential of AI in medical imaging lies in democratizing access to expert-level diagnostic capabilities. In regions with limited radiologist availability, AI systems can provide preliminary interpretations, triage urgent cases, and support non-specialist clinicians in diagnostic decision-making. Telemedicine platforms incorporating AI imaging analysis could extend specialized diagnostic services to remote and underserved communities, addressing significant healthcare equity challenges.
As algorithms become more sophisticated and validated across diverse populations and clinical settings, AI-powered medical imaging may help address the global shortage of radiologists and bring high-quality diagnostic services to populations that currently lack adequate access to specialized medical expertise.
7. Frequently Asked Questions
How accurate is AI in detecting diseases from medical images?
AI systems have demonstrated accuracy rates comparable to or exceeding expert radiologists in specific tasks such as breast cancer detection in mammograms, lung nodule identification, and diabetic retinopathy screening. However, accuracy varies depending on the specific application, quality of training data, and clinical context. Most implementations use AI as a decision support tool alongside human expertise rather than as a standalone diagnostic system.
Will AI replace radiologists?
AI is not expected to replace radiologists but rather to augment their capabilities and transform their role. While AI excels at pattern recognition and routine analysis, radiologists provide essential clinical context, integrate findings with patient history, handle complex or unusual cases, and communicate with patients and healthcare teams. The future of radiology involves collaborative intelligence between AI systems and human experts.
What types of medical imaging benefit most from AI?
AI has shown particular promise in mammography for breast cancer screening, chest X-rays for tuberculosis and pneumonia detection, CT scans for stroke and trauma assessment, retinal imaging for diabetic retinopathy, and dermatological imaging for skin cancer detection. However, AI applications are expanding across virtually all imaging modalities and clinical specialties as algorithms become more sophisticated and validated.
How do hospitals ensure AI medical imaging systems are safe and effective?
Healthcare institutions implement AI systems through rigorous validation processes, including prospective clinical studies, continuous performance monitoring, and quality assurance protocols. Regulatory agencies like the FDA review AI medical devices before market authorization. Hospitals typically maintain human oversight of AI-generated findings, establish clear protocols for system use, and conduct ongoing audits to ensure consistent performance across diverse patient populations.
What are the privacy concerns with AI analyzing medical images?
AI systems require access to medical imaging data for training and operation, raising legitimate privacy concerns. Healthcare institutions must ensure compliance with regulations such as HIPAA in the United States and GDPR in Europe. Best practices include data anonymization, secure data storage and transmission, clear patient consent processes, and limiting data access to necessary personnel. Emerging federated learning techniques allow AI training without centralized data collection, potentially enhancing privacy protections.
8. Conclusion
Artificial intelligence in medical imaging represents a paradigm shift in diagnostic medicine, offering unprecedented capabilities in accuracy, efficiency, and accessibility. Deep learning algorithms are already demonstrating clinical value across diverse applications, from cancer screening to emergency stroke detection, while addressing critical challenges facing healthcare systems worldwide.
As AI technologies continue to mature and integrate into clinical workflows, the focus must remain on thoughtful implementation that enhances rather than replaces human expertise, ensures equitable access across diverse populations, and maintains the highest standards of patient safety and privacy. The future of medical imaging lies not in competition between artificial and human intelligence but in their synergistic collaboration—combining AI's pattern recognition prowess with human clinical judgment, contextual understanding, and compassionate care.
The transformation is already underway, and healthcare organizations that strategically embrace AI in medical imaging will be better positioned to deliver higher quality, more efficient, and more accessible diagnostic services in the years ahead. As we continue to refine these technologies and address remaining challenges, AI-powered medical imaging stands poised to realize its potential as one of the most impactful applications of artificial intelligence in healthcare.

.jpg)